The overstimulation of the immune system due to COVID-19 has been found to worsen the condition of patients afflicted with the disease. Instead of fighting SARS-CoV-2 coronavirus, a hyperactive immune reaction known as a 'cytokine storm' can damage healthy cells and compound the harm caused to the body. However, researchers have developed a new blood test that can help identify patients who are at the highest risk of facing the uncontrolled onslaught of the immune system.
The study by scientists from the University of Southampton, has described a blood profile in order to test for five cytokines could that may help predict which patients are at the risk of lethal overactivity of the immune system. This can help in providing individualized treatments to patients and mitigate the damage.
"These findings, from the ongoing COVID research program in Southampton, have identified important inflammatory signals which will help steer the development of treatment strategies for this new disease," said Prof. Tom Wilkinson, lead author of the study, in a statement.
Impact of Cytokine Storms
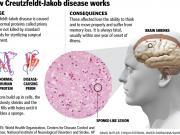
Cytokines are signaling proteins that regulate the immune system by drawing immune cells to the site of infection. However, in patients suffering from severe COVID-19, the signaling mechanism of the immune system is affected and a turbulent response known as a 'cytokine storm' damages healthy cells.
This erratic immune reaction causes injury to vital organs such as the lungs and eventually death. Therefore, identifying individuals whose risk of developing such a response is higher, and addressing the hyper inflammation may serve as an important measure in reducing adverse outcomes in COVID-19 patients.
The Four Horsemen of Cytokine Storm
For the study, the authors examined the blood samples from 100 patients who had tested positive for COVID-19 and were hospitalized at the University Hospital Southampton NHS Foundation Trust (UHS) between 20 March and 29 April 2020.
It was discovered that the increased levels of four cytokines—IL-6, IL-8, IL-1β, IL-33, and TNF—in the blood of these patients during admission has a strong connection with their chances of requiring artificial ventilation, intensive care, and increased chances of mortality. Two cytokines, in particular, IL-1β and IL-33 were found to have the largest impact.
The current study is part of a larger study led by lead author Dr. Tristan Clark— the CoV-19POC study. It is aimed at understanding the clinical effect of molecular point-of-care testing in suspected COVID-19 patients admitted at UHS. The research also includes tests that drastically reduced the time taken for the diagnosis of the coronavirus infection.
The integration of the cytokine test with proper clinical assessment of the patient's state can help doctors identify and provided treatment to those who have the biggest risk of severe outcome. Dr. Clark commented, "Our findings suggest that testing for both COVID-19 and cytokines at the point-of-care is feasible and in the future may identify infected patients and the most appropriate treatment for them, in near real-time."
Devising New Treatments
According to the authors, currently, two treatments for hospitalized COVID-19 patients said to be effective. In patients requiring oxygen supplementation, the death rates have been found to reduce by a third through the use of the steroid, dexamethasone.
The underlying mechanism of dexamethasone's protective action is unknown. However, it suggests that it may serve as a non-specific anti-inflammatory with the potential of regulating the immune system's inflammatory response.
The research team believes that the exact identification of the cytokines responsible for the hyper inflammation in individual patients may enable clinicians to target those cytokines using medications such as an IL-33 blocker used in some trials in the UK. This could also help provide individualized treatment—a concept known as 'precision medicine'.
"It is increasingly apparent that COVID is highly heterogeneous. Only by applying these techniques to stratify the condition will we be able to target the key mechanisms of disease with the best treatment for that individual," concluded Prof. Wilkinson.