In a study on prostrate cancer, researchers have found that higher levels of aneuploidy lead to much greater fatal risk among patients.
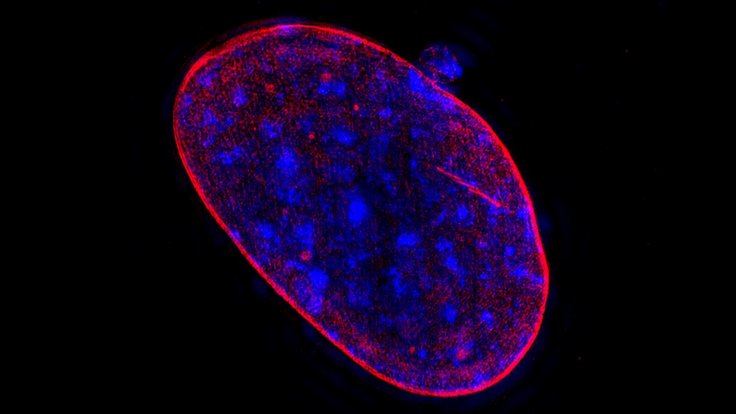
While, 23 pairs of chromosomes is considered normal in humans, any variation from this number can be fatal for cells. Biologists have known for decades that cancer cells often have too few or too many copies of some chromosomes -- called aneuploidy.
For the study, the researchers used a collection of prostate tumor samples. They had the genetic sequencing information for these samples, as well as data of whether and when their prostate cancer had spread to other organs. They were also informed if the patient had died due to the disease.
The researchers managed to calculate the degree of aneuploidy of each sample. They compared the genetic sequences of those samples with aneuploidy data from prostate genomes from the Cancer Genome Atlas, which is a documentation of data about genetic mutations responsible for cancer.
They found that patients with a higher degree of aneuploidy were five times more likely to die from the disease. The study conducted could potentially help patients' prognosis be more accurate.
Angelika Amon, Professor in Cancer Research says that this can be of aid to doctors, by providing information as to which patient must be treated more aggressively.
These findings recommend that measuring aneuploidy could offer additional information for doctors who are deciding how to treat patients with prostate cancer, Amon said, adding further that it can act as a test to help decide how to treat a patient.
"Prostate cancer is terribly overdiagnosed and terribly overtreated," Amon said. "So many people have radical prostatectomies, which has a significant impact on people's lives. On the other hand, thousands of men die from prostate cancer every year... Assessing aneuploidy could be an additional way of helping to inform risk stratification and treatment, especially among people who have tumors with high Gleason scores and are, therefore, at higher risk of dying from their cancer."
Gleason scores form a grading key which helps recognise the intensity and severity of prostrate cancer. Citing an example, a Gleason score of 6 is low grade, 7 is intermediate grade, and a score of 8 to 10 is high-grade cancer.
In short, based on the number of extra or lesser chromosomes in the cancer cell, the intensity of the treatment can be carried out.
The researchers also want to identify specific genes that might help cancer cells survive and spread, and are also studying why some prostate cancers have higher levels of aneuploidy than others. Thyroid cancer is also something they are also looking forward to study in the future.
Amon is now collaborating with Harvard T.H. Chan School of Public Health to explore whether aneuploidy can be reliably measured from small biopsy samples.
This study was published in the journal Proceedings of the National Academy of Sciences.









