Chemotherapy – administered to cancer patients for prompting their cancer cells to commit suicide – is widely used to treat various forms of cancer, but the therapy resists to work in many cases such as lung cancer for which scientists have found a pathway to treat the dangerous disease, a study says.
Researchers from the Medical College of Georgia and Georgia Cancer Center at Augusta University in their study, which sought to identify mechanisms whereby TIMP-1 impacts anticancer therapy, identified interleukin-6 (IL-6) as a key factor in chemoresistance.
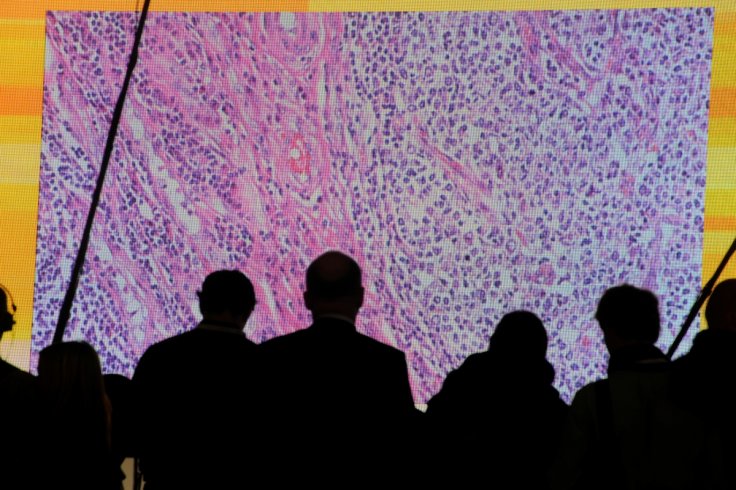
The scientists used non-small-cell lung carcinoma (NSCLC) cells and their TIMP-1 knockdown clones to examine the chemoresistance against two chemotherapeutic agents, Gemcitabine and Cisplatin, which are identified to increase apoptosis in the knockdown clones and found the exogenous human recombinant rhTIMP-1 or rhIL-6 associated with resistance to cancer chemotherapy and reduced apoptosis.
IL-6 is a sugar-coated protein that can turn inflammation both up and down and regulates TIMP-1 -- rather than vice versa -- in some cancers, but "in lung cancer, at least, it is TIMP-1 that controls IL-6", cancer biologist Dr. Mumtaz Rojiani explained.
"If TIMP-1 goes up, IL-6 goes up and if TIMP-1 goes down, IL-6 decreases ... and we have shown it in multiple different ways," said Dr. Amyn Rojiani, MCG Department of Pathology chairman and a co-author of the study published in the journal Cancers.
In the study, scientists show that TIMP-1 took the lead in avoiding cell suicide, a natural process that should happen when cells become dysfunctional and indicate that this destructive duo – TIMP-1 AND IL-6 -- may be an even more valuable indicator of a patient's prognosis and an important new target for improving it.
Rojiani said chemotherapy resistance was a big problem in types of cancers such as NSCLC, particularly when cancer recurs at which point it's also more aggressive.
To see if this tumor-promoting synergy that the researchers identified in human lung cancer cell lines also occurred in patients, they looked into the Cancer Genome Atlas database compiled by the National Cancer Institute, which includes samples and full genome sequencing from patients with a huge variety of outcomes, including chemotherapy resistance and death.
They found that patients with non-small cell lung cancer who had both low TIMP-1 and IL-6 had higher survival rates, MCG postdoctoral fellow Dr. Wei Xiao said and added that the two genes commonly elevated together, and just IL-6 elevation did not affect survival as much as just TIMP-1 elevation did.
The survival rate was much worse when both were elevated rather than TIMP-1 alone, said Mumtaz Rojiani, adding "the two-gene signature became very important."
The researchers then examined exactly how STAT3 helped in reducing apoptosis, and found active STAT3 further activated even more TIMP-1.
This is the first report of the relationship where TIMP-1 affects IL-6, which activates STAT3, in NSCLC, which is the leading cause of cancer death in both men and women and accounts for 80-85 percent of lung cancers, according to the American Cancer Society.









