Several lethal viruses such as the poliovirus and influenza viruses have become manageable due to the availability of vaccines against them. However, a vaccine to counter a virus that has led to the prevalence of a pandemic for decades still eludes scientists—HIV (human immunodeficiency virus). Offering some hope in the area of developing a vaccine against the pathogen, scientists from the Scripps Research Institute have developed a new approach that involves the use of genetically engineered immune cells obtained from the patient's body itself.
According to the study, the researchers were able to successfully induce broadly neutralizing antibodies (bnabs) that could prevent the deadly infection in a mouse model. The findings of the study have the potential to facilitate a new vaccine or an effective cure against HIV.
"People think of cell therapies as being very expensive. We're doing a lot of work towards trying to make the technology affordable as a preventative HIV vaccine or functional cure that would replace daily antiviral therapy," said Dr. James Voss, principal investigator of the study, in a statement.

No Known Cure
A cure for HIV has been a sustained pursuit for the scientific community for decades. According to the World Health Organization (WHO), nearly 38 million people are living with HIV across the world as of 2018. It can affect individuals of any age. The infection spreads through contact with the body fluids of an infected person. It could be through sexual contact, or through other means such as from mother to fetus or through blood transfusion.
As the infection progresses, it can lead to the development of acquired immunodeficiency syndrome (AIDS), where the immune system of the body becomes fragile and incapable of defending the body. This leaves it vulnerable to other infections and diseases.

Patients suffering from the viral infection are treated using combination antiretroviral therapy (cART). It involves a treatment regimen that employs three or more antiretroviral drugs and is aimed at reducing the replicating capacity of the virus. Also, other than following precautionary measures, there are no medical options available to prevent the contraction of the disease.
Engineering A Patient's Own Cells
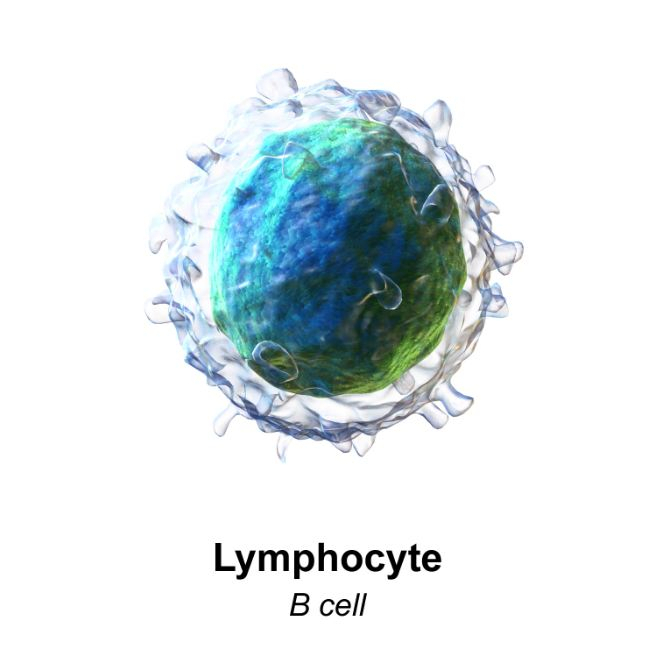
In 2019, Voss and his team demonstrated that antibody genes of the B lymphocytes, a type of white blood cells, which are also known as B cells, can be reprogrammed using the gene-editing technique CRISPR. The cells were programmed to generate the broadly neutralizing HIV antibodies that are found in extremely rare HIV patients. In the current study, the team strived to illustrate the results of reintroducing the engineered cells into the body.
Using a mouse model, the study showed that these engineered B cells, upon being reintroduced into the body, can increase in numbers in response to vaccination. They could mature into plasma and memory cells that had the ability to give rise to elevated levels of protective antibodies for extended periods of time within the body.
Additionally, the authors are also proved that genes that have been engineered can be further improved in order to manufacture antibodies that are highly effective against HIV pathogen. For this, a naturally occurring process in the B cells that is initiated in response to immunization could be leveraged, the scientists said. "This is the first time it has been shown that modified B cells can create a durable engineered antibody response in a relevant animal model," explained Voss.
According to Voss, the cells required to produce the vaccine can be obtained from human beings simply by drawing blood from a patient. Then, they can be engineered and introduced into the patient again. The team is now reviewing methods in which the technology can be improved and be made accessible to large sections of the population.









