Medical resources are stretched thin in megacities so much so that the healthcare administrators are faced with the uneasy task of giving preferential treatment to patients who have higher chances of recovery. And this is not as simple as it sounds - it's a morally challenging task that involves the decision to deny life-saving equipment to some patients on the death bed. The 'Ventilator Triage' issue the authorities and health experts in New York are discussing is a case in point.
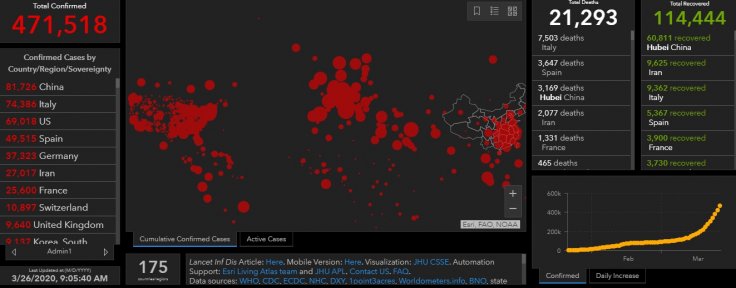
Coronavirus has spread to 198 countries with 471,794 confirmed cases and 21,297 deaths reported globally, posing new problems to the countries already struggling to contain the virus and keep the death rate under check. Metropolises like New York, Madrid and Milan are creaking under the load of medical emergencies, while cities like London are bracing for the worst. Dearth of crucial equipment like ventilator and even protective gear for the medics is a problem health authorities are facing everywhere.
What is Ventilator Triage?

Ventilator is a crucial equipment in treating a patient with coronavirus as this disease deals with respiratory problems. Triage is the assignment of degrees of urgency to wounds or illnesses to decide the order of treatment of a large number of patients or casualties. In the case of treating patients with coronavirus, the hospitals and health centres are facing severe shortage of ventilators around the world. This has led to the concept of 'ventilator triage' and here is how countries, especially the US is fighting the cause.
Hospitals rationing care and equipment
Hospitals have more critically ill patients suffering from coronavirus than the equipment available to treat them. Thus, hospitals are planning to ration care and equipment to save as many people as possible. General guidelines in this regard are being provided to hospitals across the US, including points system being developed to determine if the patient should live or die.
Taking such a tragic decision has become a necessity, especially in countries where death rate runs into hundreds per day with thousands of cases being confirmed daily.
As per 'Ventilator triage', priority is being given to those most likely to be saved, and most likely to live longer. Ethics committees in the health sector are working hard to provide a solution and recently, Halpern and Dr Douglas White, chairman of ethics in critical care medicine at the University of Pittsburgh, released guidance to hospitals in this regard to hospitals in the US.
What is a point system? What are the parameters?
They described a points system where critically ill patients are rated from 1 to 8. Patients with high chance of survival get less rating starting from 1 and those already suffering from diseases like cancer, dementia or chronic illness and have less chances of survival are placed with high numbers.
The guidance also places critically ill patients in need of ventilators into four age categories: 12 to 40; 41 to 60; 61 to 75; and older than 75. But as always age cannot be used as a parameter for greater chance of survival for a COVID-19 patient, there is contemplation about appointing an independent arbiter apart from the in-charge physician so that decisions of allotting ventilators is not biased and doesn't put pressure on the doctor treating the patient, who has to decide if the patient should live or die.
However, those who do not get the ventilator facility will surely receive other ICU facilities including symptom management and, palliative care.
Removing ventilator is equal to killing the patient
Another challenge after placing a patient on the ventilator is the decision to withdraw it if the patient does not respond to treatment. In the US, 50 years ago, the opinion was that removing ventilator is equal to killing the patient and was banned in terms of law too. But currently, withdrawal of ventilator system is the most common form of death in unavoidable situations. However, this decision is taken by the attending physician or the surrogate.
But in the case of COVID-19 patients, this option cannot work as it is a difficult situation for a physician and family members and as there is no time to be wasted as another person with high chance of survival may die due to delay in decision making. Hence it is necessary that a third party (not attending to patients) is asked to make the decision so that large number of people are saved with timely decision.
Dire situation in New York

Citing the seriousness of the problem of ventilator shortage, New York Governor Andrew Cuomo said that there are only 6,000 ventilators operating in New York and it is woefully inadequate to handle the situation. He also said that his appeal had responses like FEMA sending 400 ventilators. "You pick the 26,000 people who are going to die because you only sent 400 ventilators," he told expressing helplessness and anger.
Another report in "The New England Journal of Medicine" suggests that currently, acute care hospitals in the United States have nearly 62,000 fully functioning ventilators and 98,000 basic ventilators. It said that there are also additional 8,900 ventilators in the Office of the Assistant Secretary for Preparedness and Response Strategic National Stockpile.
However, even this number of ventilators is insufficient as up to 31 patients will have one ventilator considering the surge in cases of coronavirus in the US.
Thus rationing of ventilators and medical care by a triage committee with no clinical responsibilities with regard to any patient only can provide unbiased decision and might save a large number of people suffering from coronavirus.









