For people struggling with certain types of cancer, immunotherapy—a treatment that helps the immune system fight cancer—can serve as a life-saving intervention and result in improved prognosis. However, scientists from the University of Toronto have identified dozens of genes that enable cancer cells to evade the immune system and avoid getting killed, thereby presenting a major challenge in cancer treatment.
Through the study, the authors found over 180 genes whose presence affecting immune actions. "It's very important to understand at the molecular level how cancer develops resistance to immunotherapies in order to make them more broadly available. Advances in systematic genetic approaches have let us key in on genes and molecular pathways that are commonly involved in resistance to therapy," said Jason Moffat, lead author of the study, in a statement.
A Life-Saving Treatment
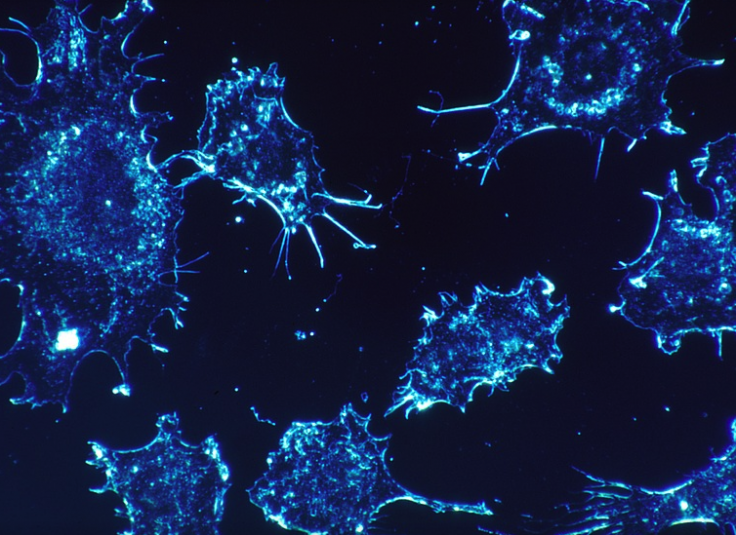
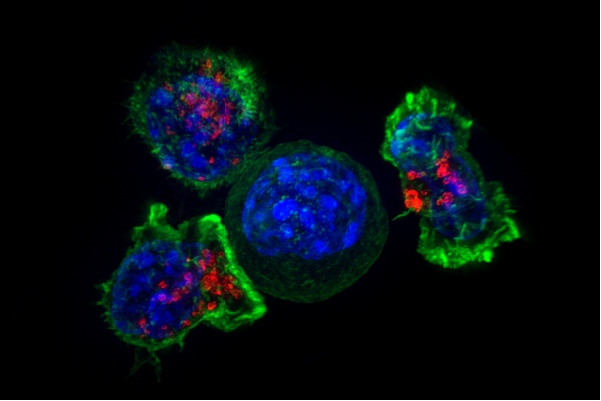
Immunotherapy is a therapeutic management procedure where a patient's own immune cells, particularly cells known as T killer cells, are engineered to seek and destroy cancer cells. Unfortunately, resistance to the treatment renders it ineffective in several patients, especially those battling solid tumors.
Also, tumor heterogeneity is another challenge that complicates cancer treatment. It is the genetic variation in tumor cells among themselves, and also among different individuals. "Over the last decade, different forms of immunotherapy have emerged as really potent cancer treatments but the reality is that they only generate durable responses in a fraction of patients and not for all tumor types," said Moffat.
Identifying Role of Genes In Immune Evasion
For the study, the scientists scouted for genes that promoted immune evasion across six genetically varying tumor models obtained from kidney, colon, skin, and breast cancer. The chosen cancer cells were deposited along with T cells designed to seek out and destroy them, in a Petri dish. Also, the activity or 'attack' of the T cells serves as the baseline.
Next, the authors utilized CRISPR—a gene-editing tool—to deactivate the genes of the cancer cells one-by-one. They measured the difference in the activity of the T cells against the modified cells and compared them to the baseline measurements.
Discovery of Dozens of Essential Genes
The gene omission yielded unexpected results. A staggering 182 "core cancer intrinsic immune evasion genes", whose deletion either made the cancer cells ward off T cell attacks or increased their sensitivity to them, were identified. Among the resistant genes were those who are known to mutate and render immunotherapy ineffective in patients.
Surprisingly, several of the identified genes had no known links evasion of immune functions. "That was really exciting to see, because it means that our dataset was very rich in new biological information", said Keith Lawson, co-lead author of the study.
Using the Body's Defences Against It
Autophagy is a process where the cells clear out dysfunctional or unrequired components and enable regeneration of new and healthy cells. However, genes involved in the process presented themselves as a key in the evasion mechanism. This also provided the scientists with the idea of magnifying the weakness of cancer cells against immunotherapy by supplementing the treatment with drugs targeting these specific genes.

Nevertheless, as the researchers investigated the gene further, they discovered that the omission of certain autophagic genes in pairs made the cancer cells resistant to the onslaught of T cells. This meant that if a tumor already possesses a mutation in an autophagy gene, the combination of immunotherapy and a gene suppressing drug could lead to disastrous outcomes in patients.
"We found this complete inversion of gene dependency. We did not anticipate this at all. What it shows us is that genetic context, what mutations are present, very much dictates whether the introduction of the second mutations will cause no effect, resistance or sensitivity to therapy," explained Moffat.
Devising New Effective Therapies
The authors also stated that new therapies must factor in the dangers posed by the mutations—referred to as cancer resistance mutations—in tumors because treatments aimed at their elimination may potentially worsen the disease in patients.
"It's important to not just find genes that can regulate immune evasion in one model of cancer, but what you really want are to find those genes that you can manipulate in cancer cells across many models because those are going to make the best therapeutic targets," stressed Lawson.